The National Center for Child Health and Development has successfully performed the world’s first transplant of human ES cell-derived hepatocytes into a human. What is the potential of these cells, which saved a small life, to bring great happiness?
The infant patient had urea cycle dysregulation, in which one of the liver’s enzymes is absent, resulting in elevated ammonia levels in the body. In many cases, the condition can cause infants to suffer serious brain injury as a side effect, or even to die immediately after birth. And for technical reasons owing to their small bodies and organs, liver transplants are normally difficult to perform on such newborns. In this case, NCCHD transplanted an HAES, a therapeutic agent derived from ES cells for hyperammonemia, to the baby and succeeded in improving the liver function temporarily until the baby’s weight reached 6kg, the minimum weight required to achieve a liver transplant safely. Five months later, the baby received a liver transplant from its father and was discharged from the hospital without any complications.
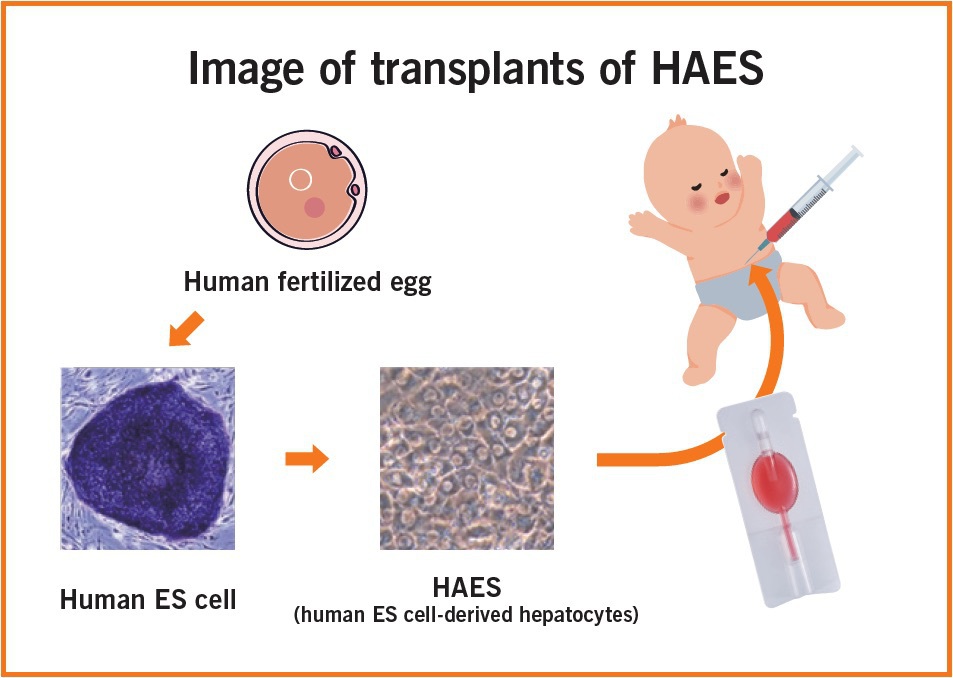
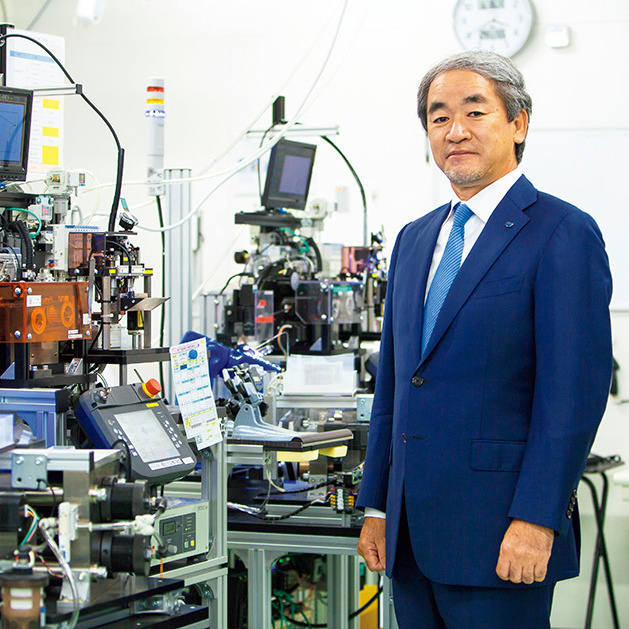
Dr. KASAHARA Mureo, the doctor in charge of the surgery, explains the benefits of this treatment as follows: “We were able to save a life that couldn’t have been saved before. In many previous cases, patients with this disease used to undergo liver transplants only after further damage had occurred, but with the new treatment, neither disabilities nor complications result from the disease. In the treatment, we injected the HAES via the bellybutton, enabling us to carry out the operation while barely scarring the baby’s body.”
The ES cells that make the treatment possible are pluripotent stem cells generated from a human fertilized egg. Such cells, which have drawn much attention recently for their potential in the field of regenerative medicine, have the distinctive feature of being able to differentiate into any type of cell, as well as to propagate indefinitely. Moreover, because of their unlimited proliferative potential, the same cell can be created and distributed repeatedly. It is for this reason that ES cells are rigorously regulated in terms of bioethics and safety. The NCCHD is one of only two institutions in Japan permitted to establish ES cells.
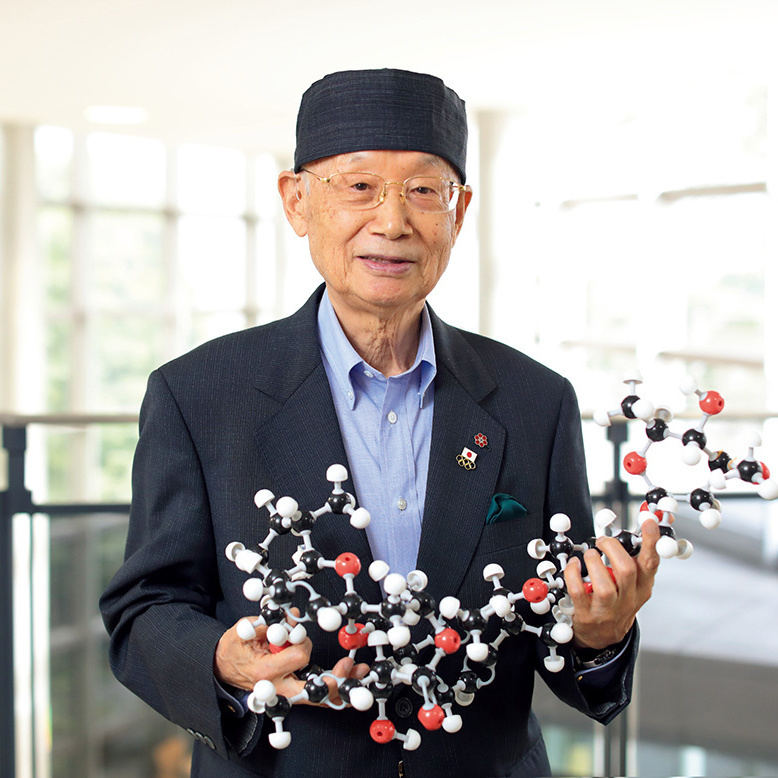
Another doctor at the NCCHD, Dr. UMEZAWA Akihiro, successfully used ES cells to generate hepatocytes that are highly functional in lowering ammonia concentration; that was what led to the transplant this time. Dr. Umezawa has this to say about the future of ES cells: “The possibilities of ES cells are unlimited. Of course, that means it is even more important to proceed with caution, care, and transparency. We must be able to deal with each patient individually, while maintaining the same quality. As we move forward, we would like to explore a wide range of applications and promote collaboration with other medical institutions.”
Dr. Kasahara, in charge of the latest transplants, is a specialist in pediatric liver transplants, having performed more than 1,500 such operations around the world. He says, “Nothing could be so wonderful as seeing regenerative medicine expand in the future to include fulminant hepatitis, liver cirrhosis, and hemophilia, and restoring those patients to health without their needing organ transplants. That might cause me, however, to lose my job.”
News of the operation’s results quickly spread all over the world, and already, the NCCHD has received requests for joint research and clinical consultations from such countries as the United States, Canada, the United Kingdom, and India. An endeavor to save one small life born in Japan has thus opened new doors for medical treatment.

Dr. KASAHARA Mureo, executive director of the Organ Transplantation Center, was in charge of the operation. He says, “To be able to treat patients while preserving their quality of life is even more meaningful when one considers what it means to their family and to society.”

Dr. UMEZAWA Akihiro, director of the Center for Regenerative Medicine, was in charge of HAES production. He says, “I am hoping that ES cells will offer breakthroughs for the many patients for whom effective treatment or medicine has yet to be found.”

The National Center for Child Health and Development was established to facilitate coordination between the hospital and laboratory for the advanced medical treatment of diseases related to the reproduction cycle, from fertilization and pregnancy through to adulthood.