Masayo Takahashi
Dr. Masayo Takahashi graduated from Kyoto University’s Faculty of Medicine in 1986. In 1992, she completed her Ph.D. in Visual Pathology at Kyoto University’s Graduate School of Medicine. She first worked as a clinician, but later became interested in research following her studies in the United States in 1995. In 2005, her lab became the first in the world to successfully differentiate neural retina from embryonic stem cells. She is currently the project leader of the Laboratory for Retinal Regeneration at the RIKEN Center for Developmental Biology (CDB).
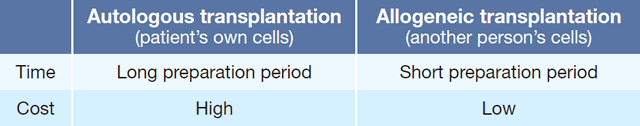
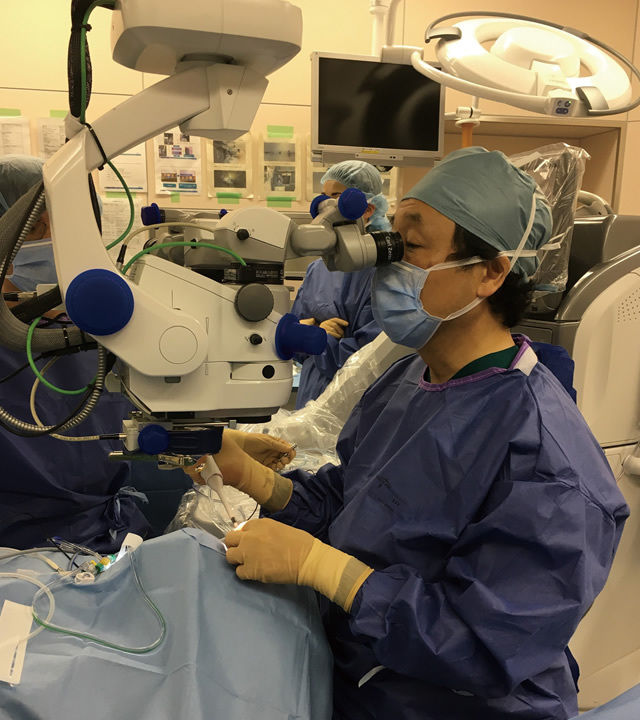
In September 2014, a team led by Dr. Masayo Takahashi, Japan’s leading ophthalmologist, of the Japanese research institute RIKEN carried out the world’s first induced pluripotent stem cell (“iPS” cell) transplant surgery for an eye disease. The generation of iPS cells was first announced in 2006 by Professor Shinya Yamanaka, the director of Kyoto University’s Center for iPS Cell Research and Application (CiRA). These cells are capable of differentiating into various cell types that make up the tissues and organs in the body, and are believed to have potential uses in restoring cells lost by sickness or injury, bringing hope of providing cures to diseases for which there was previously no treatment. The iPS cell transplant surgery conducted by Dr. Takahashi and her team has garnered much attention as a remarkable achievement that is anticipated to lead to practical regenerative medical applications.
“My interest in regenerative medical research began,” explains Dr. Takahashi, “when I accompanied my husband in his studies abroad in the United States and learned of the existence of stem cells that were capable of replenishing cells in the body. Although I was later successful using embryonic stem cells to produce retinal cells, I knew as soon as I heard about the discovery of iPS cells that I’d found the ideal stem cell. I credit our world’s-first achievement to being specialized in the clinical field of ophthalmology while also being exposed to stem cell research, which was a completely different field, and also to the fact that we’ve always kept pushing our research forward on the leading edge.”
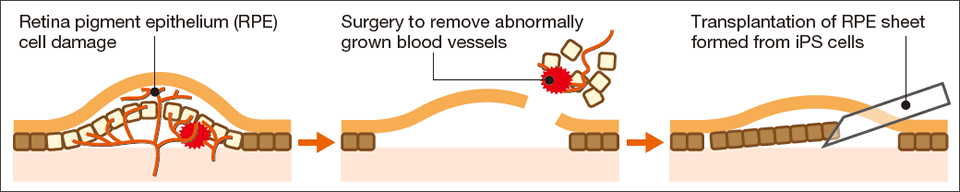
In the above-mentioned surgery, iPS cells were made from the skin tissue of a patient who was suffering from wet-type age-related macular degeneration (AMD), and these iPS cells were differentiated into retinal pigment epithelial (RPE) cells and processed into the form of a cell sheet. The RPE cell sheet was then transplanted into the patient from whom the iPS cells were generated, which was able to prevent further deterioration of the patient’s eyesight (a symptom of wet-type AMD).